Do you start itching when you eat cured meat? What about random headaches you can’t figure out? Or perhaps your tongue gets all swollen when you eat bananas?
If you’ve answered yes to any of these questions, let me assure you that it’s not ‘all in your head’: you could have a histamine intolerance. Or more precisely a ‘mast cell activation disorder’. I’ve experienced histamine intolerance first hand, which is why I wrote this article. So I know how annoying and troubling the symptoms can be.
But the good news is that you can get better. Read on to find out everything you need to know about histamine intolerance and what you can do to address the root cause of your symptoms.

What is histamine?
What comes to your mind when you think of histamine? Allergies and a stuffy nose during seasonal changes? Or perhaps the redness and painful swelling caused by a mosquito bite or a bee sting? Well, these symptoms occur due to the release of histamine, an organic nitrogen compound that causes an immediate inflammatory response.
Many of us see histamine as an irritating bad guy that causes allergies. But the truth is that histamine is a normal physiological response that acts as a red flag to alert the body of any potential attacker.
Moreover, histamine also works as a:
- Neurotransmitter which communicates important messages between the brain and various parts of the body.
- Component of stomach acid which helps the body extracts nutrients from the food you eat.
Immune system meets Invader – a real life story
The production of histamine is very complex but in a nutshell, here’s how that goes:
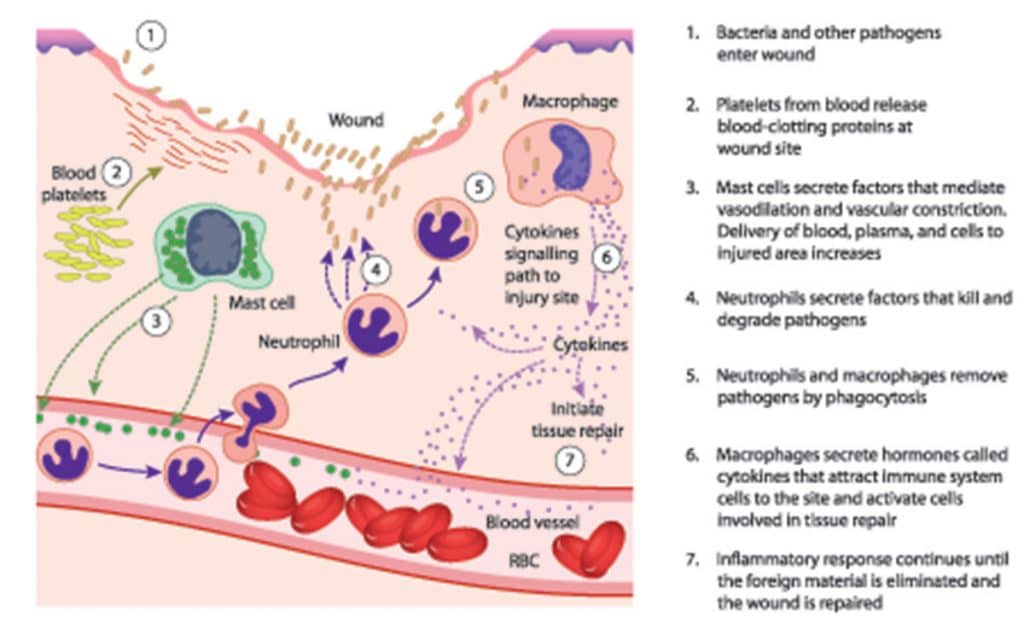
1. An invader (such as pollen, dust particles or an insect’s venom) enters the body.
2. The immune system encounters the invader and trigger mast cells, white blood cells that act as the sentinels of our innate immune system.
3. The mast cells quickly notify the body by releasing histamine from secretory granules (storage sacs).
4. The histamine produced triggers the release of other immune cells and also dilates capillaries – small blood vessels. This swelling makes the capillaries more permeable to those immune cells, allowing them to quickly find the invader and attack it.
5. Usually, once the invader has been ‘apprehended’, the body releases two main enzymes. These include namely histamine N-methyltransferase (HMT or HNMT) and diamine oxidase (DAO). HMT and DAO break down the histamine produced into N4-methylhistamine and imidazole acetaldehyde respectively. These reactions inactivate the histamine thus preventing its accumulation in the blood.
For most people, this usually marks the end of the story. However, as discussed below, for some individuals, histamine can be a much greater issue.
[color-box color=”main”]Good to know: Bacteria in our guts also produce histamine. Plus, some of the foods we eat contain histamine. And to make things more confusing, some foods can trigger the release of histamine.[/color-box]
 Histamine intolerance – Not your typical food intolerance
Histamine intolerance – Not your typical food intolerance
Let me start by saying that, just like ‘adrenal fatigue’, ‘histamine intolerance’ is a collection of symptoms and not a diagnosis. This is why many conventional practitioners will tell you that histamine intolerance does not exist.
A mast cell activation disorder (MCAD) is currently the most accurate diagnosis of what patients with ‘histamine intolerance’ are suffering from. However, since not many individuals know about MCAD, I’ll be using the term ‘histamine intolerance’ in this article.
As mentioned earlier, mast cells act as the guards of the immune system. Therefore, in an attempt to maintain a normal environment within the body, these cells react to changes in the environment or insults to the body. They do so by releasing molecules such as histamine. For optimal body function, we need these mast cells and the molecules they release. Besides their role in allergies, mast cells are involved in:
- The production of new blood cells
- Wound healing
- Immune tolerance development
- Maintenance of the blood-brain barrier function
- Protection against pathogens
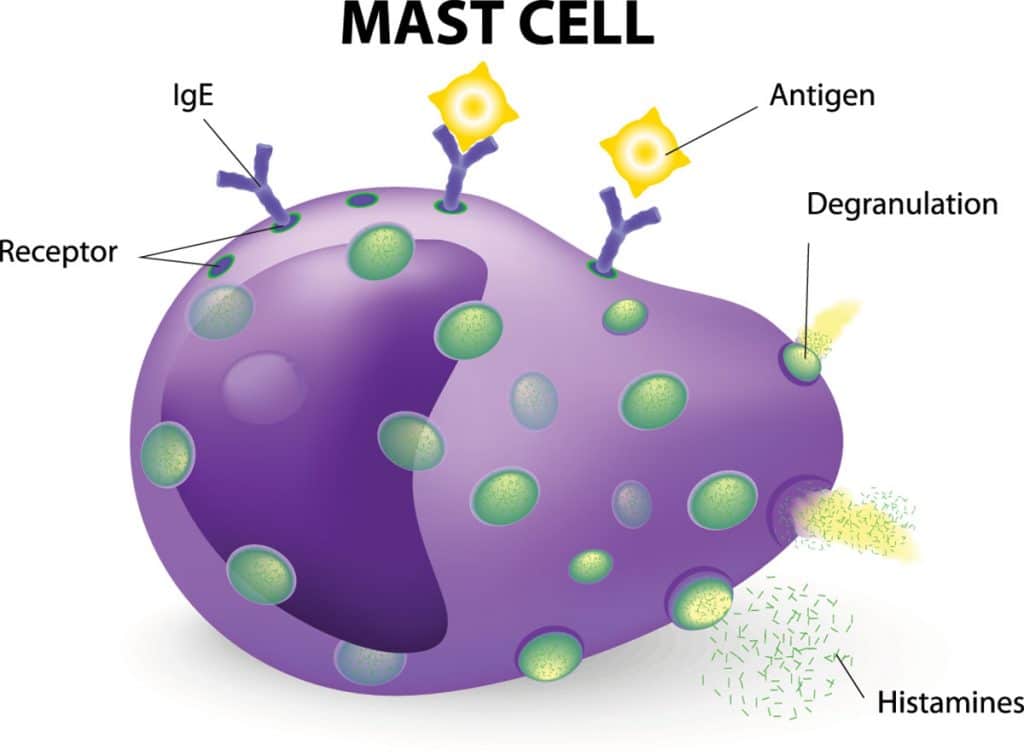
However, in the case of MCAD, problems occur when these cells function abnormally, leading to histamine intolerance. MCAD has also been linked to:
- Skin conditions
- Irritable bowel syndrome (IBS)
- Depression and anxiety
- Alzheimer’s disease
- Obesity
- Diabetes
- Male infertility
- Autoimmune disorders like rheumatoid arthritis
- Bladder pain syndrome
[color-box color=”main”] Good to know: Although MCAD can be ‘in your genes’, different members of the same family can present with very different symptoms.[/color-box]
Why would someone have issues with histamine?
By now, you will have realized that the problem isn’t with the histamine. So why would histamine be so problematic for some individuals?
Well, based on current research, it appears that some individuals produce too much histamine whilst others are unable to break down histamine.
Why would a person make too much histamine?
1. Overactive mast cells (mast cell activation syndrome). This can be caused by:
– Toxicity of heavy metals like aluminum and mercury
– Infections or gut dysbiosis
– Chronic Inflammatory Response Syndrome (CIRS) – individuals who are particularly sensitive to molds, are more likely to be constantly activating their mast cells. That’s because these individuals would be less able to clear out mycotoxins (poisons released by toxic molds) from their bodies.
4. Mastocytosis, a rare genetic condition caused by an excess of genetically altered mast cells.
3. Too many gut bacteria that produce histamine.
Why would a person have trouble breaking down histamine?
Unfortunately, there are numerous possibilities. For instance, a person may suffer from:
- A deficiency of histamine N-methyltransferase (HMT or HNMT)
- Impaired efficiency of DAO due to genetic mutations in the DAO gene. These mutations are more common among Caucasians.
- Reduced activity of HMT due to micronutrient deficiencies which can affect the methylation pathway through which HMT deactivates histamine
- Low levels of bacteria that degrade histamine
- MTHFR mutation – No, it’s not a swear word (although it sure looks like one!): MTHFR actually stands for methylenetetrahydrofolate reductase. This involves a defect in the genes related to the methylation pathway. Individuals who are homozygous for MAO can be more sensitive to histamine. [A 23andMe gene profile run through Genetic Genie or MTHFR Support can help you determine this.]
Some individuals may also be deficient in diamine oxidase (DAO). This deficiency can be caused by:
- A genetic issue with DAO production (more common in people of Asian origin)
- Gluten intolerance
- Increased intestinal permeability (very common among individuals on a standard Western diet)
- Inflammation
The following drugs can also interfere with DAO levels in the body:
- Non-steroidal anti-inflammatory drugs like aspirin or ibuprofen
- Antihistamines like Zyrtec, Allegra and Benadryl
- Histamine (H2) blockers like Tagamet, Zantac, Pepcid
- Antidepressants like Cymbalta, Effexor, Prozac, Zoloft
- Immune modulators like Plaquenil
- Antiarrhythmics like metoprolol
Why does the degree of histamine sensitivity vary so much?
That’s a question I get asked all the time. Some may say that a person suffering from poor health or poor lifestyle habits is more likely to be more histamine intolerant. While it is true that health status does determine sensitivity, the issue is much more complex.
For instance, one could have a MAO mutation coupled with ineffective methylation and trouble breaking down histamine once it is produced. Plus, they could have overactivated mast cells that lead to histamine overproduction. And all this could happen even if that person is eating a real food diet and practicing a healthy lifestyle.
So, there are cases where there is a constellation of issues. As such, these people may need to always be careful with foods rich in histamine.
[color-box color=”main”] Good to know: If you must talk to your doctor about histamine intolerance, use the term ‘mast cell activation disorder’ instead. Otherwise, she/he might look at you like you have two heads.[/color-box]
Common symptoms of histamine intolerance
Symptoms will vary considerably (from irritating to life-threatening) between individuals depending on which body systems are affected:
- Eyes – Redness, itching, burning, watery
- Nose – Runny, itching, sneezing, seasonal allergies
- Mouth – Swelling, itching
- Skin – Swelling, rashes, itching, hives (can be localized or all over the body)
- Throat – Swelling or ‘throat tightening’
- Lungs – Coughing, wheezing
- Digestive tract – Heartburn, indigestion, reflux, cramps, diarrhea
- Vascular – Headaches, fatigue, confusion, irritability, symptoms resembling those of anxiety or panic attack, loss of consciousness unexplained by other causes
- Cardiovascular – Drop in blood pressure (especially when you stand up quickly), chest pain, increased heart rate or ‘racing heart’
[color-box color=”main”] Take-home message: Since all human tissues contain mast cells and almost every cell has a mast cell receptor, MCAD can affect any organ system, making detection quite difficult.[/color-box]
Now that you know what histamine intolerance is, let’s talk about how to test for it.

Testing for histamine intolerance
1. Elimination / Reintroduction diet: Start by eliminating foods rich in histamine, those that release histamine as well as DAO blocking drinks (see below) for at least 30 days. Then, work with a qualified healthcare practitioner to reintroduce foods one at a time.
2. Blood tests: Test for both histamine and DAO levels. Moreover, you can also run a serum tryptase test to assess mast cell activation syndrome.
Usually, a high histamine to DAO ratio would indicate that your:
- Dietary intake of histamine is too high (if you’re on a normal diet)
- Body is over-producing histamine (due to gut dysbiosis) on a low-histamine diet
- Body isn’t producing enough DAO levels.
But if your DAO levels are very low and you have normal histamine levels, then that could indicate a genetic deficiency of DAO.
3. DAO supplements: If you are unable to test your histamine and DAO levels, you could do a ‘DAO supplement trial’. You just have to eat a low histamine diet and take a DAO supplement at each meal. If your symptoms improve, this could indicate that you have low DAO levels.
Histamine-free and low histamine diet
If you do a Google search for ‘histamine intolerance’, you’ll come across the ‘histamine-free’ or ‘low histamine’ diet, a VERY long list of foods to avoid. I have to admit that just glossing through foods to avoid on a low histamine diet can be quite distressing. Netherveless, this diet is an important part of treatment as it can help you tone down some of your symptoms and finally get relief.
Let’s have a look at foods which naturally contain histamine, those that release histamine and those that inhibit DAO.

Histamine-rich foods
As the name suggests, these foods contain histamine. The biggest offenders are usually any type of fermented foods – during fermentation, the bacteria produce histamine. Leftover meat can also be problematic since microbial action increases histamine levels as the meat sits. Slow cooked foods like bone broth or crockpot recipes will also be high in histamine.
- All fermented alcoholic beverages especially wine (white and red), beer, champagne, sherry and all other alcoholic drinks – even if the alcohol has been cooked off
- Cured meats including bacon, dried cured sausages, hot dogs, luncheon meats, pepperoni and salami
- Pork
- Smoked or canned seafood and seafood that has been improperly handled or stored for too long
- Certain fish like anchovies, bonito, butterfly kingfish, dried milkfish, herring, mackerel, mahi-mahi, marlin, pilchards, saury, scads, smooth-tailed trevally
- Tuna and sardines – the amount of histamine varies between different species with some containing no histamine at all
- Fish paste (like anchovy paste), fish paste and shrimp paste
- Fermented foods like kefir, kombucha, sauerkraut, yogurt, fermented sausages, fermented ham, vinegar, soy sauce and any fermented soy product
- Vinegar-containing foods such as mayonnaise, pickles, and preserved olives
- Soured-foods like buttermilk, soured bread, sour cream, and sour milk
- Dried fruits like apricots, dates, figs, raisins, prunes
- Most citrus fruits
- Nuts like cashews and walnuts
- Peanuts
- Cheeses like Camembert, cheddar, Emmental, Gouda, Harzer (German sour milk cheese), Parmesan, Swiss cheese and Tilsit or Tilsiter cheese
- Avocados
- Coffee
- Eggplant
- Pineapples
- Spinach
- Strawberries
- Tomatoes and ketchup
[color-box color=”main”] Did you know? The average histamine content of the above foods can vary between 2mg/kg to 400mg/kg! Fruits are usually lower in histamine compared to cured meats, pork, and sausage which win the award for foods highest in histamine. [/color-box]
Histamine-releasing foods
The following foods do not contain histamines. However, when ingested, they can trigger mast cells to release histamine.
- Alcohol
- Bananas
- Chocolate
- Cocoa
- Cow’s milk
- Crustaceans
- Licorice root
- Nuts
- Papaya
- Pineapple
- Pork
- Shellfish
- Tomatoes
- Wheat germ
- Various artificial preservatives and dyes
DAO-Blocking beverages
As the name suggests, in susceptible individuals, the following drinks can inhibit DAO’s activity when consumed
- Alcohol
- Black tea
- Green tea
- Mate tea
- Energy drinks
That’s a long list of foods but, don’t worry, once you’ve addressed the root cause of your histamine intolerance, you’ll probably be able to start enjoying them again.

So what can you eat?
As a rule of thumb, when it comes to histamine intolerance, remember to eat the freshest foods you have access to:
- Freshly cooked poultry, meat and game
- Cooked eggs
- Fresh produce excluding avocado, eggplant, spinach, tomatoes
- Dairy substitutes like coconut or almond milk
- Extra virgin olive oil and virgin coconut oil
- Herbal teas
- Certified gluten-free rice, quinoa, buckwheat and amaranth – avoid these if you have an autoimmune condition or a lot of inflammation in your body (this would be indicated by high ESR and/or CRP levels on blood tests)
- Freshly caught fish – the video below will walk you through how to select the freshest fish
Do you really need to address your root cause?
Short answer: Definitely!
Because do you think you could follow a low-histamine diet for life? If yes, that’s impressive! However, be forewarned: not this only can this diet be very overwhelming, but it may not be very useful in the long run if you don’t address the underlying cause.
Why? For two main reasons:
- A low-histamine diet with supplemental DAO will only help reduce the amount of histamine that you’re consuming. It will do nothing to modify the amount produced by your mast cells within your body.
- No two individuals with histamine intolerance will react to the same foods. For instance, my dad gets hives when he eats spinach but no reaction whatsoever when he eats eggplants, unlike my older brother who reacts strongly to eggplants. In other words, if you avoid all foods that contain histamine, you will probably be missing out on foods you may actually tolerate well.
Plus, to make things more complicated, the histamine content of foods will vary depending on:
- How they’ve been handled
- Processing methods
- The type of bacteria that has been used in fermentation
This is one of the reasons why you won’t find histamine content on labels.
Why not simply follow conventional treatments?
Conventional treatments involve drugs that focus on blocking the action of mast cell mediators like histamine. It is true that they can give you much-needed relief but these short-term solutions can have unwanted side effects.
This is why I strongly advise addressing the root cause of your histamine intolerance. While this will not be a quick fix, this approach can help you reverse your condition.

So, how can you treat histamine intolerance?
1. Heal your gut!
If you’ve read my previous articles, you’re probably thinking ‘Whoa, what a broken record!’ But the importance of a healthy gut cannot be over-emphasized. You see, histamine intolerance indicates both a damaged gut (increased intestinal permeability) as well as an overgrowth of bad bacteria and too few beneficial ones (dysbiosis).
To heal your gut, avoid:
- Gluten-containing foods
- Grains
- Vegetable oils (like canola oil, cottonseed oil, sunflower oil, safflower oil and soybean oil)
- Sugar
- Processed foods.
You can also try probiotics but adhere closely to these two guidelines:
- Avoid probiotics that produce histamine – these can worsen your symptoms. Hello chaos if they start colonizing your gut! These probiotics include Lactobacillus bulgaricus, Lactobacillus casei and Lactobacillus delbrueckii. These strains are often found in most dairy products which is why I strongly discourage consumption of fermented dairy products if you have histamine intolerance.
- Try probiotic strains that degrade histamine – these should improve your symptoms. Lactobacillus plantarum and Bifidobacterium infantis are good choices. Or you could try soil-based organisms.

2. Give your liver some love
Remember HMT, the other enzyme that breaks down histamine? Well, it is active in the liver. If your liver is unhealthy, the efficiency of HMT will decline. So, to keep your liver healthy, you want to:
- Avoid sugar and high fructose corn syrup
- Choose healthy fats (such as coconut oil) instead of refined, industrial seed oils
- Select nutrient-packed carbohydrates such as sweet potatoes
- Eat a colorful diet to get enough polyphenols
- Be active throughout the day to use up your liver glycogen stores
- Avoid alcohol – this includes wine – since it is one of the major inhibitors of DAO
3. Take care of any existing infections
As mentioned earlier, parasites and infections can over-activate mast cells. Your doctor can work with you to assess your comprehensive stool test analysis and identify what might be bugging you.

3. Take care of any existing infections
This test will help determine if you are suffering from heavy metal toxicity. Once you get the test’s results, try chelating agents (under the guidance of a qualified healthcare professional) to get rid of these metals. It is also a wise idea to have a trained dentist safely remove any old mercury fillings you may have. This can reduce the burden of mercury on your body.
Lifestyle changes to improve histamine intolerance
1. Get enough quality sleep
Activation of mast cells tends to be similar to circadian rhythms. As such, hit the hay early and get enough sleep (about seven to eight consecutive hours at night) is essential. You also want to avoid blue light from electronic devices at night. This being said, if you really need to use such devices at night, install f.lux on your laptop or Mac or twilight on your smartphone. Moreover, take care of your circadian hygiene by getting enough sunlight exposure on a daily basis, whenever that’s possible.
2. Manage your stress levels
When you’re stressed (physically or physiologically), your body releases corticotropin hormone. This hormone ‘startle’ mast cells, causing them to release mediators such as histamine. Hence, this is why many individuals will see symptoms worsen during periods of stress. You may also want to try some supplemental magnesium. But be sure to know how to select the right magnesium supplement for you.

Nutrients to include
1. Resistant starches
These include unripened green bananas – these are great in smoothies or fried in coconut oil to make chips. But make sure to avoid raw potato starch which may worsen your symptoms. That’s because lectins, naturally occurring substances in potatoes, can provoke mast cells to release histamine.
2. Get plenty of nutrients that can help stabilize your mast cells
Here’s what I typically use in my practice:
- Bromelain (natural anti-histamine)
- Butterbur
- Ginger
- Holy basil
- Nettle tea
- Nigella sativa
- Peppermint
- Pine bark extract (natural anti-histamine)
- Quercetin (natural anti-histamine)
- Selenium
- Thyme
- Turmeric
- Vitamin C from amla berries or camu-camu
Have you experienced histamine intolerance? If so, what was your underlying issue and what did you do to address that?